Having a digital repository of healthcare information at hand could improve care, enhance collaboration and increase efficiency. A survey of Indian hospitals revealed that health information systems were available and used routinely in most facilities, despite wide variation in their capabilities. While most hospitals shared data internally, the majority were unable to utilise digital patient data generated within other hospitals.
Why Measure Health Information System Use
In March 2018, the Ministry of Health and Family Welfare issued a draft of the Digital Information Security in Healthcare Act (DISHA). The proposed law would establish national and state electronic health authorities to monitor collection of digital health data. Among its many features, it would give autonomy to patients to choose whether or not they would like to have their information digitally recorded. In order to put the importance of this law into context, it is helpful to understand the degree to which Indian hospitals are already digitally using and storing patient data.
The recent success of Practo, an India-based personal health record and physician appointment scheduling app, has sparked curiosity about the use of health information technology (IT) in India. As the market leader in the space, Practo has seen a number of notable competitors such as Lybrate. More broadly, the digitisation of physician appointment scheduling has served as an entry point for new technologies into the Indian healthcare system. Nonetheless, Indian healthcare is still very much in flux. Organisations in the sector vary widely in their adoption of health information systems. What do the data say about the use of information systems within Indian hospitals? We conducted a survey of hospitals to answer this question.Our survey offers relevant insights for this emerging area of policy development. By understanding the capabilities of the health information technologies in use, vendors can also better understand the desires, needs, and readiness of the marketplace for new solutions. Among our key findings: physician resistance remains an important barrier to health information systems adoption, alongside the perceived lack of inter-operable IT systems in the Indian marketplace. That said, in our sample, at least some IT functionalities, such as digital access to patient demographics, was reported to be available and used by the majority of the respondents. While health information exchange within the organisation was well-established, exchange of information to coordinate care with external providers was weak.
Understanding Health IT in India
Researchers from many countries have sought to understand the extent to which health IT is being used by hospitals. While there have been some one-off national level studies of health IT adoption in various countries, there is a need to develop international standards to characterise health IT. The Organisation for Economic Cooperation and Development (OECD) formulated a generalised survey for assessing health IT adoption within member nations in 2016. This survey, titled “Draft OECD Guide to Measuring ICTs in the Health Sector”, is intended for use in countries with diverse healthcare systems, whether substantially public, such as in the United Kingdom (UK) or substantially private, such as in the United States (US). The 2016 data from the International Monetary Fund shows that members of the OECD also have a wide range of incomes, spanning from Luxembourg’s Gross Domestic Product (GDP) per capita on a Purchasing Power Parity (PPP) basis of $98,987 to Mexico’s $17,534. While India is not a member of the OECD and has a somewhat lower GDP per capita of $6,162 compared to member nations, the OECD’s survey can be implemented in India with only minor modifications.
The scale and diversity of India can make conducting a representative national survey difficult. However, even surveys using unrepresentative samples can be used to better understand pockets within India that have embraced health IT. Identifying such pockets enables Indian companies to confidently enter the domestic health IT market, knowing that there are some customers available. Likewise, highlighting exemplars can inspire hospitals which are yet to adopt health IT.
In order to characterise potential exemplars, the Max Institute of Healthcare Management at the Indian School of Business (ISB) commissioned two surveys using an adapted version of the OECD’s survey instrument. The OECD survey was supplemented with a series of questions related to barriers to adoption of IT in healthcare. These questions were borrowed from a survey of American hospitals administered by Jha and co-authors in an article published in 2009. For the pilot study, hospitals affiliated with the ISB Healthcare Management Programme were surveyed on the use of health IT within their facilities. The hospitals were asked to complete an online questionnaire and in the event of omissions, were contacted to ensure completeness.
The pilot survey included 30 respondents, 93% of whom were based in cities with over 100,000 inhabitants. The majority of the respondents (13) were from Hyderabad. New Delhi was represented by three respondents, and the remaining came from a variety of other Indian cities. The majority reported that their facility was private or corporate. The respondents’ facilities tended to be medium or large. Only 10% of respondents reported their facility had 6-99 beds, while 55% reported 100-399 beds, and 34% reported 400 or more beds. Inpatient (IPD), outpatient (OPD), and emergency care were nearly universally available at the hospitals. Only one respondent reported the lack of an inpatient department and only two respondents reported the lack of an emergency department.
Digital Health Information Storage
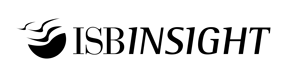
Some IT provisions were available in the majority of the hospitals. Only one respondent reported the lack of an IT system to store and manage patient information. Hospitals were then asked how frequently specific types of information were stored and used – routinely, occasionally, not used, or not available.
As Figure 1 shows, a wide range of features was reported to be available and used at least occasionally by the majority of the hospitals. Capabilities for storing patient demographics were most likely to be available and used routinely, while electronic systems for recording immunisations were the least likely to be available. These findings suggest that while hospitals lacking all of the surveyed features were in the minority, the hospitals varied widely in the extent to which they used the features in everyday practice.
To place these numbers in context, by 2015, 83.8% of US non-federal acute care hospitals had basic electronic health records (EHRs), capable at the minimum of storing patient demographics, problem lists, medication lists, and discharge summaries (Henry, Pylypchuk and Patel 2016). These EHRs also allowed for the computerised ordering of medications and facilitated the electronic viewing of laboratory, radiology and diagnostic test reports. The adoption of these features occurred rapidly. Only 16.1% of these US hospitals possessed the functionality six years prior, when the government subsidised adoption through the 2009 Health Information Technology for Economic and Clinical Health (HITECH) provisions in the in the American Recovery and Reinvestment Act.
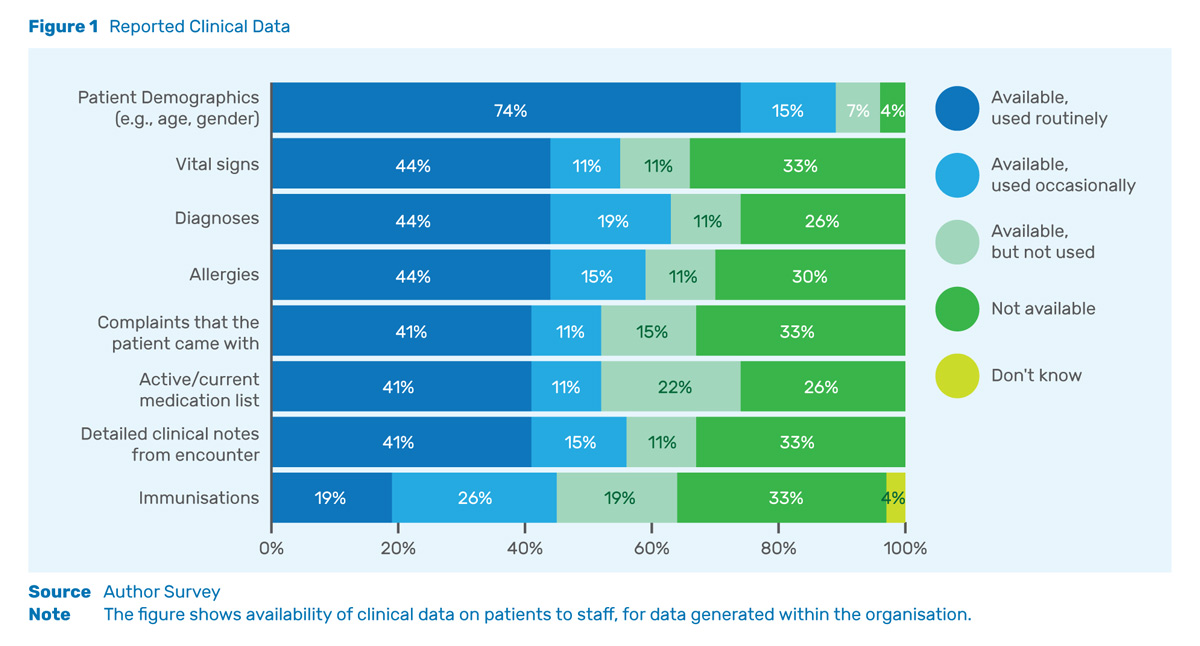
The most common intra-organisational data sharing features currently available revolve around ancillary services – radiology and laboratory results. These results are electronically shareable and used routinely.
Internal Information Exchange Capabilities
Sharing data between departments within a hospital is another important use of health information systems. As is shown in Figure 2, the most common intra-organisational data sharing features currently available revolve around ancillary services – radiology and laboratory results. These results are electronically shareable and used routinely in the majority of the organisations surveyed. Capabilities related to sending electronic referrals and patient summaries were less likely to be available or used routinely. This suggests that the focus in electronic systems to date has been on enabling providers to receive the results of diagnostics that they have ordered, instead of enabling them to collaborate with other physicians.
External Information Exchange Capabilities
Patients may need to receive care at multiple hospitals if a single hospital lacks the capabilities to fully address a health condition, or if patients maintain multiple residences. Hospitals must share information with each other if the care for such patients is to be coordinated. Currently, there is a gaping lack of digital inter-organisational inter-operability in India, which is largely filled by patients transporting their own records on paper between facilities. Indian healthcare faces the same situation as the US, which has also struggled to foster inter-operability (Adler-Milstein 2017).
According to our survey, less than half of the hospitals were able to receive health information when it was generated outside the organisation. Patient demographics were the most likely to be available, with 48% reporting availability and 33% reporting that externally-generated patient demographics were used routinely. In contrast, 33% of organisations reported receiving information pertaining to allergies, immunisations, and vital signs were from external sources.
Non-federal acute care hospitals in the US faced similar challenges, albeit to a lesser degree. In 2015, 85% reported being able to send information to other facilities and 65% reported being able to receive it. Routine use of external information was likewise an issue in the US. According to a 2016 report by Patel and co-authors, only 18% of hospitals reported that they often used external information, while 35% reported that they sometimes did so.
Pro-active Care and Population Health Management
The future of the digitisation of inpatient and outpatient care in India will revolve around electronic prescribing and order entry. When physicians prescribe medications or procedures by clicking checkboxes instead of writing on a sheet of paper, a computerised decision support system can analyse whether there are potential errors in the prescriptions and make evidence-based recommendations to improve care. Among the hospitals surveyed in the pilot, 37% reported that electronic prescribing was not available. Only 33% reported that it was used routinely. When electronic prescribing was available, prescriptions were only sent within the organisation. No hospitals reported sending prescriptions to pharmacies outside the hospital. Patient safety will depend upon electronic prescribing becoming ubiquitous.
When physicians prescribe medications or procedures by clicking checkboxes instead of writing on a sheet of paper, a computerised decision support system can analyse whether there are potential errors in the prescriptions and make evidence-based recommendations to improve care.
Although all of the features related to pro-active care mentioned on the survey were in use by at least one hospital, their use was far from universal. Alerts related to allergies were reported as available by 40% of respondents, while alerts related to drug interactions were reported as available by 36% of respondents. As hospitals upgrade their information systems, many may be able to extract greater clinical benefits from the information that they have already collected by introducing these information-based features.
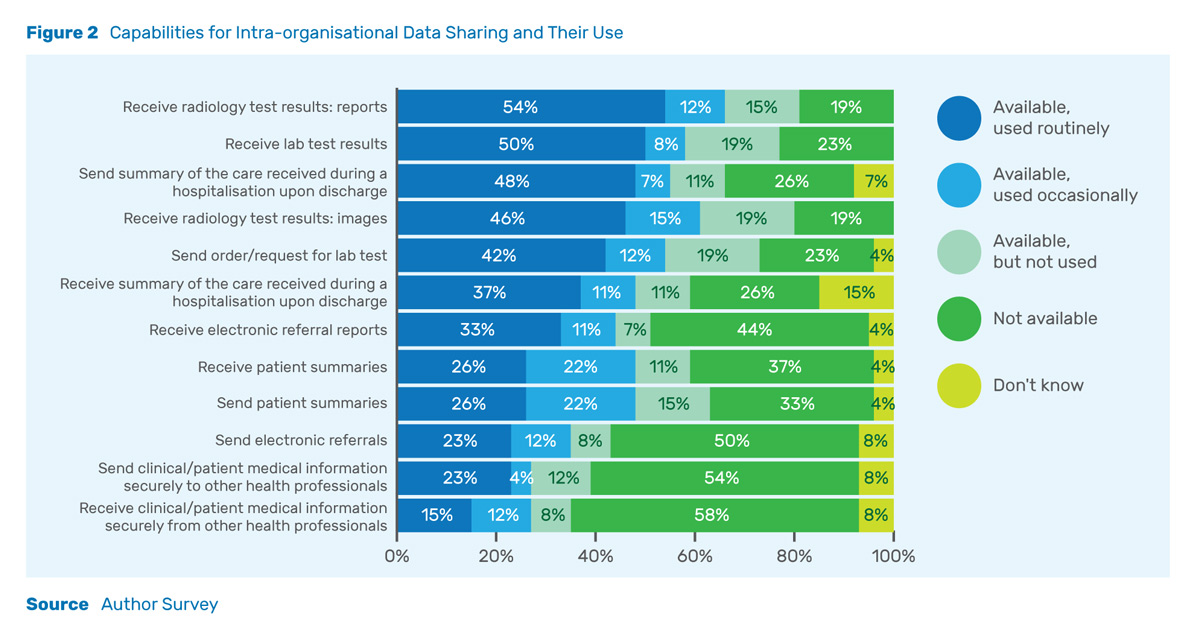
Digital prescribing and record-keeping enable hospitals to manage populations of patients before they enter the hospital. When hospitals can list patients by diagnosis, determine patients in need of tests, or view a comprehensive list of the medications patients are taking, physicians can reach out to patients, encouraging them to receive necessary care. While traditionally, physicians have waited for patients to remember to return for follow-ups visits, software identification of gaps in care can increase the likelihood that patients will get the care they need while boosting hospital revenue.
While Indian hospitals largely operate on a fee-for-service basis, limited population health management tools appear to be available. Population health management—working to improve the health outcomes of groups rather than individuals—makes financial sense when hospitals are paid capitated rates to care for populations or when it can be used to increase the volume of care delivered.
Among the respondents, 48% reported that they were able to electronically list patients due for tests. This feature can be used to both drive fee-for-service revenue and in the future, to manage populations. Figure 3 depicts the availability of a number of functions related to population health management. From the survey, it is clear that a number of hospitals have the functionality necessary to begin addressing care on a pro-active, rather than a reactive basis. In general, there appears to be greater digitisation of the laboratory than the pharmacy.
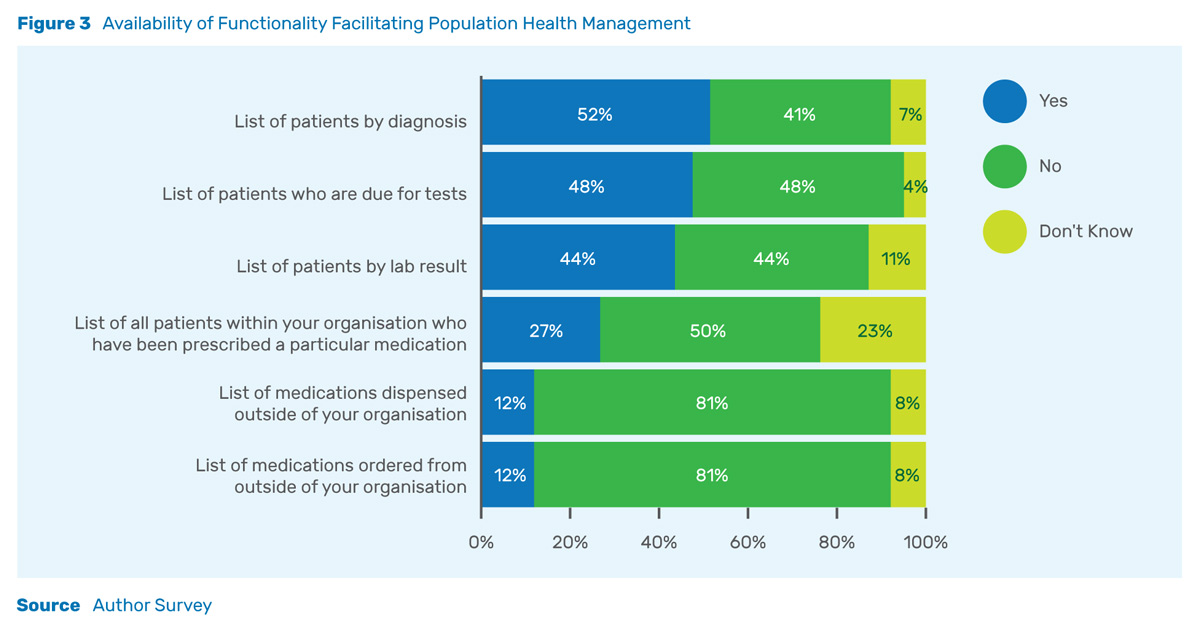
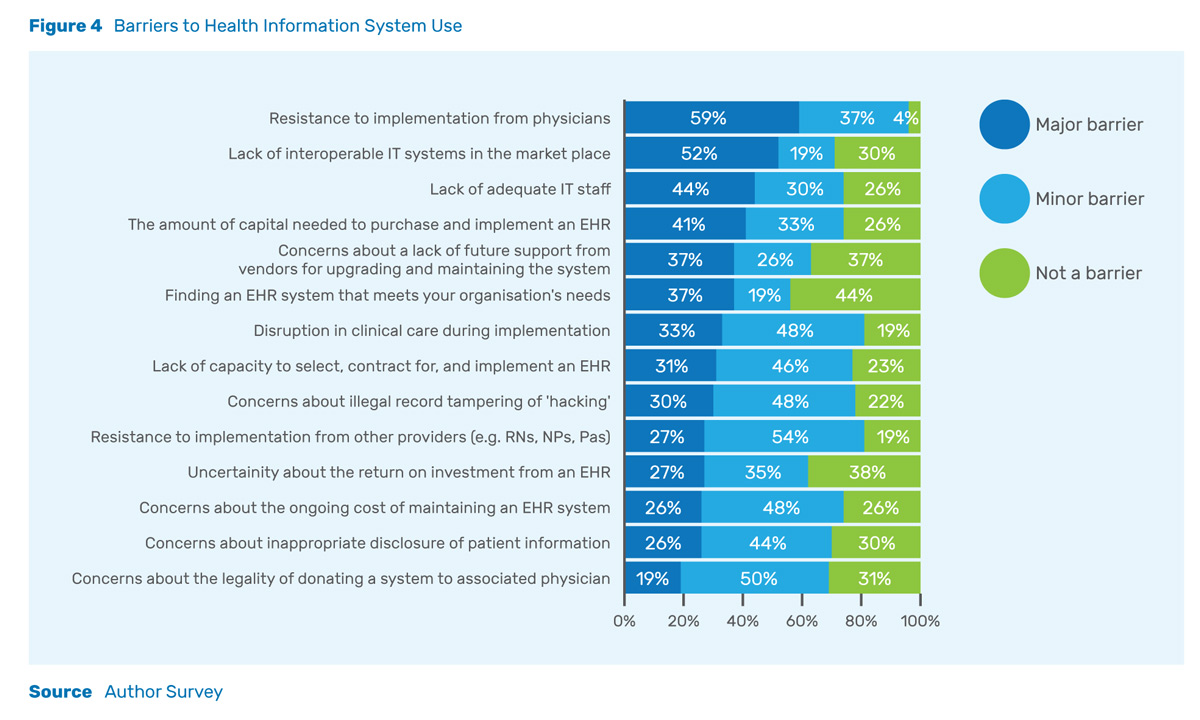
Among those who implemented health information systems, the top barrier reported was resistance from physicians. The second most frequently reported major barrier was a lack of inter-operable IT systems in the marketplace.
In the US, 70% of physicians were electronically prescribing drugs in 2014. This was a ten-fold increase over the only 7% electronic prescribing rate in 2008. Legislative changes in the US in 2009 and 2010 transformed electronic prescribing from a novelty to the norm (Gabriel and Swain 2014). This suggests that with the right incentives or regulations, electronic prescribing can be rapidly adopted.
Barriers to Implementation
Many hospitals have begun the process of implementing health information systems. However, several of them have faced challenges along the way. As Figure 4 shows, among those who implemented health information systems, the top barrier reported was resistance from physicians (59%). The second most frequently reported major barrier was a lack of inter-operable IT systems in the marketplace (52%). Both commercial and privacy concerns were reported by less than half of respondents. Commercial concerns included concerns over initial capital expenditures (41%), return on investment (27%), and ongoing costs (26%). Privacy concerns included concerns over hacking (30%) and inappropriate disclosure of patient information (26%). Facilities with commercial concerns may have had difficulty linking the potential for enhanced efficiency or quality resulting from health IT with greater profitability.
Organisations that did adopt IT felt that internal resistance and the options externally available to them were greater barriers than capital or security. This suggests that system vendors need to educate the market to allay concerns from both physicians and from purchasers. The development of local standards or greater adoption of international standards may reduce concerns over inter-operability.
One of the drivers of digitisation in the US has been changes in payment arrangements between hospitals and insurers. Population health management has become increasingly important in the US. This has happened as insurers have moved hospitals towards value-based contracts which combine fixed capitation payments based upon the number of patients treated (capitation) with quality metrics (for more, see Feldman et al 2016). Measuring and improving quality requires detailed data.
Future Directions
There is a common perception that India makes little use of health IT. The adoption of EHRs was subsidised in the US through the HITECH provisions in the American Recovery and Reinvestment Act of 2009, in Canada through initiatives by Canada Health Infoway, and in the UK by the National Health Service (NHS) National Programme for IT. In India, the Ministry of Health and Family Welfare introduced Electronic Health Record (EHR) standards in 2013, but there was little legal backing for enforcement of these standards. Furthermore, the utility gained from electronic health records may be lower in India, as patients tend to retain comprehensive paper records of their care, whereas in the US, such records have traditionally resided with the physician rather than the patient. Thus, Indian patients have been able to coordinate information between healthcare providers in a way which is not possible in the US.
Just as the HITECH provisions led to a health IT renaissance in the US, it is possible that a new regulation, such as DISHA, may do the same in India. In less than a decade, health IT went from being a novelty to a norm in US hospitals. That being said, the level of health IT adoption reported by our survey respondents was more advanced on several measures than was seen in US before the HITECH provisions were instituted in 2009. Given the right incentives and regulations, a similar transformation could occur in India.
Know More
Adler-Milstein, J., 2017. Moving past the EHR interoperability blame game. NEJM Catalyst.
Chauhan, R. and Kumar, A., 2013. Practo Technologies: the online way of life! Emerald Emerging Markets Case Studies, 3(7), pp.1-19.
Feldman, K., Stiglic, G., Dasgupta, D., Kricheff, M., Obradovic, Z. and Chawla, N.V., 2016. Insights into population health management through disease diagnoses networks. Scientific Reports, 6 (30465).
Gabriel M, Swain M. 2014. E-prescribing Trends in the United States. The Office of the National Coordinator for Health Information Technology, ONC Data Brief, 18.
Henry, J., Pylypchuk, Y. and Patel V., 2016. Electronic capabilities for patient engagement among US non-federal acute care hospitals: 2012-2015. The Office of the National Coordinator for Health Information Technology.
Henry, J., Pylypchuk, Y., Searcy, T. and Patel, V., 2016. Adoption of electronic health record systems among US non-federal acute care hospitals: 2008-2015. The Office of National Coordinator for Health Information Technology.
Jha, A.K., DesRoches, C.M., Campbell, E.G., Donelan, K., Rao, S.R., Ferris, T.G., Shields, A., Rosenbaum, S. and Blumenthal, D., 2009. Use of electronic health records in US hospitals. New England Journal of Medicine, 360(16), pp.1628-1638.
Patel, V., Henry, J., Pylypchuk, Y. and Searcy, T., 2016. Interoperability among US Non-Federal Acute Care Hospitals in 2015. ONC Data Brief, 36, p.36.
Powell, Adam C., Ludhar, Jasmine K and Ostrovsky, Y., 2017. “Electronic health record use in an affluent region in India: Findings from a survey of Chandigarh hospitals.” International Journal of Medical Informatics, 103 (2017), pp. 78-82.